Do you have an elderly parent or other loved one who spends most of their day in bed? If so, they may be increasingly vulnerable to developing a pressure ulcer (or “bed sore”), which is a type of skin injury that can happen when an individual remains in the same position for too long. It’s important to know what these injuries look like and how to spot them early on so that treatment can begin right away – this blog post will guide you through everything you need to know about recognizing pressure ulcers, including signs, symptoms, and prevention tips.
Definition of a Pressure Ulcer or Bed Sore
A pressure ulcer, more commonly known as a bed sore, is an injury that can occur when the skin and underlying tissue experience prolonged pressure or friction against a surface. These wounds are particularly prevalent in individuals who have limited mobility and are unable to change positions frequently enough to relieve pressure on vulnerable areas. Pressure ulcers can range in severity, from a mild discoloration of the skin to an open wound that extends deep into underlying tissue. Treatment for pressure ulcers usually involves keeping the affected area clean and dry, changing positions frequently, and ensuring proper nutrition and hydration to promote healing. Early detection and timely intervention are key to preventing serious complications, such as infection or tissue damage.
Types of Pressure Ulcers
Pressure ulcers are a common skin injury, occurring when there is prolonged pressure on a particular area of the skin. These ulcers can range in severity, from mild to severe, and are classified into different types based on their location and appearance. The most common types of pressure ulcers are stage 1, which is characterized by redness and minor skin irritation; stage 2, which involve the formation of blisters or open sores; stage 3, which involves deeper tissue damage; and stage 4, which involve the most severe tissue damage and can extend into muscle and bone. Proper prevention and treatment of pressure ulcers are crucial in promoting overall skin health and preventing further complications.
– Grade I (mildest form)

Grade I, also known as the mildest form, is a commonly used terminology in the medical world to describe the severity of certain conditions. For instance, a concussion can come in various grades, with Grade I being the least severe. This grading system helps healthcare professionals determine the appropriate treatment plan for the patient. It’s important to note that while Grade I may be mild, it still requires prompt medical attention to avoid potentially worsening symptoms. If you or someone you know experiences any concerning symptoms, always seek medical attention right away.
– Grade II
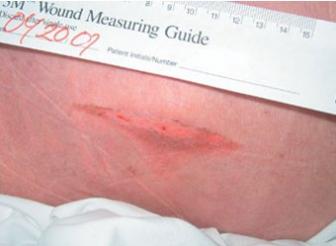
Grade II pressure ulcers present as a shallow open sore with a red-pink wound bed, without slough. They may also present as an intact or ruptured serum-filled blister.
– Grade III

Grade III pressure ulcers are deep crater-like sores that extend into the subcutaneous tissue. The wound bed will appear yellowish and have slough and/or necrotic tissue present. The edges of the wound may be undermined, rolled or hard.is an important stage in a student’s educational journey.
– Grade IV (most severe form)

Grade IV is the most severe form of its kind. When it comes to medical conditions, reaching the fourth stage is never a good sign, and this is certainly no exception. Whether we’re talking about tumors or another type of ailment, it’s a diagnosis that sounds scary and can feel overwhelming for those affected. But understanding the specifics of what it means can help guide important conversations between patients and medical professionals. While the road ahead may not be easy, it’s important to focus on education and communication to make informed decisions and create a treatment plan that works for each case.
Symptoms and Signs of A Pressure Ulcer
Pressure ulcers, also known as bedsores or pressure sores, are common skin injuries among individuals who have limited mobility due to illness or injury. These wounds occur when an area of skin is under constant pressure and is not relieved, reducing the blood flow and causing tissue damage. Symptoms of a pressure ulcer may include redness, swelling, soreness, and a warm sensation in the affected area. As the wound progresses, it may turn into a blister or an open sore, making it susceptible to infection. It is essential to identify the warning signs of a pressure ulcer early to prevent the wound from worsening. Proper wound care, repositioning, and pressure relief can help manage pressure ulcers and promote healing.
Causes and Risk Factors for Developing A Pressure Ulcer
Pressure ulcers, also known as bedsores, are a serious medical concern that can develop when an individual spends prolonged periods lying or sitting in the same position. While anyone can develop a pressure ulcer, certain individuals are at a higher risk. Those with limited mobility, such as those who are wheelchair-bound or bedridden, are especially susceptible. Additionally, individuals with medical conditions that affect blood flow or cause decreased sensation, such as diabetes, are at a higher risk. Other factors, such as poor nutrition, dehydration, and smoking, can also increase the risk of developing a pressure ulcer. Caregivers and individuals with limited mobility need to be aware of these risk factors and take measures to prevent pressure ulcers from developing.
How to Prevent Pressure Ulcers in At-Risk Patients
Pressure ulcers, also known as bedsores, can be a significant concern for at-risk patients. These sores develop due to constant pressure on the skin, leading to tissue damage, and can be painful and difficult to treat. The best way to prevent pressure ulcers is to take proactive measures that reduce pressure on the affected areas of the body. This includes changing positions frequently, maintaining proper personal hygiene, and using specialized cushions and mattresses that distribute weight evenly. Regular skin inspections can also help identify and treat pressure ulcers in their early stages. These preventive measures are essential for helping patients at risk of developing pressure ulcers to avoid unnecessary pain and complications.
Treatment Options for Pressure Ulcers
Pressure ulcers, also known as bedsores, are a common problem faced by people who spend prolonged periods in bed or are wheelchair-bound. These wounds can be challenging to treat, and untreated ulcers can lead to life-threatening complications. Thankfully, there are various treatment options available for pressure ulcers. One option involves relieving pressure on the affected area by repositioning the patient regularly. Another involves using dressings and ointments to encourage healing. In more severe cases, surgery may be necessary. It’s crucial to seek medical attention promptly if you or a loved one develops a pressure ulcer to prevent further complications. With proper care and treatment, pressure ulcers can heal, and the quality of life can improve for those afflicted.
Pressure ulcers, also known as bed sores, are common and potentially dangerous medical conditions. Individuals need to know about the various types and grades of pressure ulcers and how to spot them early to treat them before they become worse. Various risk factors can increase a person’s likelihood of developing them, but through preventative measures such as maintaining proper hygiene and frequent repositioning, people can minimize the chance of developing these sores. Additionally, if a patient is already suffering from a pressure ulcer there is a wide range of treatment options available such as dressings, topical agents, debridement, oxygen therapy, nutrition support, and surgery. Individuals need to be mindful of the risk factors associated with these ulcers to safeguard themselves from developing moderate or severe cases that could cause tremendous complications. Educating family members on best practices concerning caring for elderly relatives can go a long way in reducing instances of negligence in nursing homes causing pressure sores as well. If you would like to learn more about nursing home negligence and its impact on elderly patients with pressure sores, subscribe below!
Signup to receive more information and special offers!